PCOS in Women:
PCOS in Women:
Polycystic Ovary Syndrome (PCOS) is a complex endocrine disorder affecting approximately 1 in 10 women of reproductive age. It is one of the most common causes of hormonal imbalance in women and a leading contributor to infertility, metabolic dysfunction, and psychosocial distress. Despite its prevalence, PCOS often goes undiagnosed or mismanaged, highlighting the importance of early recognition and evidence-based intervention.
What is PCOS?
PCOS is a heterogeneous condition characterized by ovarian dysfunction, hyperandrogenism (elevated male hormones), and polycystic ovarian morphology on ultrasound. It is classified under functional hypothalamic-pituitary-ovarian axis disorders, with systemic implications that extend beyond reproductive health.
Etiology and Pathophysiology
The exact cause of PCOS remains multifactorial and not fully understood. However, major contributing factors include:
- Genetic predisposition
- Insulin resistance (up to 70% of cases)
- Hyperinsulinemia, which stimulates ovarian androgen production
- Chronic low-grade inflammation
- Hypothalamic-pituitary axis dysregulation
This hormonal imbalance disrupts follicular maturation, leading to anovulation and the formation of multiple small cysts in the ovaries
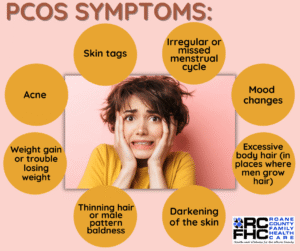 Common Signs and Symptoms
Common Signs and Symptoms
Women with PCOS may present with one or more of the following:
- Menstrual Irregularities
(oligomenorrhea, amenorrhea, or irregular cycles) - Hyperandrogenic Features
(hirsutism, acne, male-pattern baldness) - Polycystic Ovaries on pelvic ultrasound
- Infertility or subfertility
- Weight gain, especially central obesity
- Acanthosis nigricans (indicative of insulin resistance)
- Mood disturbances and increased risk of depression and anxiety
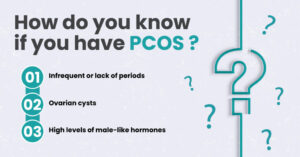
Diagnosis: Rotterdam Criteria (2003)
Diagnosis requires at least two of the following three criteria:
- Oligo- or anovulation
- Clinical/biochemical signs of hyperandrogenism
- Polycystic ovaries on ultrasound
Exclusion of other disorders such as congenital adrenal hyperplasia, thyroid dysfunction, or androgen-secreting tumors is essential.
 Medical and Lifestyle Management
Medical and Lifestyle Management
Management of PCOS is symptom-targeted and often multidisciplinary.
1. Lifestyle Modification
- First-line intervention in all patients
- Includes caloric control, regular exercise, and weight loss
- Even a 5-10% reduction in body weight can restore ovulation and improve insulin sensitivity
2. Pharmacological Treatment
| Symptom/Concern | Recommended Therapy |
|---|---|
| Menstrual irregularities | Combined oral contraceptives (COCs) |
| Hirsutism/Acne | Anti-androgens (e.g., spironolactone, cyproterone) |
| Insulin resistance | Metformin |
| Infertility | Letrozole (first-line ovulation induction agent) |
Note: Clomiphene citrate, once a standard, is now second-line to letrozole in ovulation induction.
3. Monitoring and Prevention
- Annual screening for type 2 diabetes, dyslipidemia, and cardiovascular risk
- Mental health support for anxiety, depression, or body image issues
- Consideration of endometrial protection in cases of prolonged anovulation to prevent hyperplasia
Conclusion
PCOS is more than a reproductive disorder — it is a lifelong metabolic and hormonal condition that requires comprehensive, individualized care. Early diagnosis, informed lifestyle changes, and targeted medical therapy can significantly improve quality of life and reduce long-term complications. Awareness and proactive management are essential for empowering women affected by this silent yet impactful syndrome.